Ovulatory dysfunction refers to irregular or absent ovulation, which can significantly impact fertility. Ovulation is the process by which an egg is released from the ovary, a complex event regulated by precise hormonal signals between the brain and ovaries.
The pituitary gland, located at the base of the brain, plays a key role in this process by releasing two essential hormones:
If pregnancy does not occur, the corpus luteum naturally resolves after approximately two weeks, causing estrogen and progesterone levels to fall and triggering a period.
If pregnancy does occur, the corpus luteum is sustained by rising levels of the pregnancy hormone (hCG). It continues to produce estrogen and progesterone, which are essential for maintaining the pregnancy until the placenta takes over hormone production.
This intricate balance of hormones underscores the importance of diagnosing and addressing any disruptions that may interfere with ovulation and fertility.
When these hormonal signals are disrupted, ovulation may not occur regularly, making conception more difficult.

Menstrual cycles that are longer than 35 days, shorter than 21 days, or entirely absent (amenorrhea) may indicate irregular or absent ovulation. This occurs when hormonal signals from the brain to the ovaries are disrupted, preventing the normal release of an egg.
Excessive bleeding (menorrhagia) or very light periods (hypomenorrhea) can reflect hormonal imbalances affecting ovulation. These imbalances may alter the growth of the uterine lining, leading to abnormal bleeding patterns.
Trouble becoming pregnant after trying for several months may suggest an underlying issue with ovulation. Regular ovulation is essential for conception and if this is inconsistent or absent, it reduces the chances of the egg being available for fertilisation.
Signs such as persistent acne, excessive hair growth in areas like the face or chest (hirsutism), or thinning hair on the scalp may point to conditions like Polycystic Ovarian Syndrome (PCOS) or other hormonal disorders that interfere with ovulation.

PCOS is a common hormonal disorder that disrupts ovulation due to elevated levels of androgens (male hormones.) It can cause irregular periods and other symptoms like weight gain and excess hair growth.
Hypothyroidism (underactive thyroid): Can lead to hormonal imbalances that interfere with ovulation.
Hyperthyroidism (overactive thyroid): Can also lead to hormonal imbalances that interfere with ovulation.
Excess prolactin (the hormone responsible for milk production) can suppress ovulation by disrupting the balance of reproductive hormones.
A condition where ovarian function declines before the age of 40, leading to irregular or absent ovulation.
Chronic stress can elevate cortisol levels, which may suppress the release of hormones needed for ovulation.
Overtraining or intense physical activity can lead to energy deficits and hormonal disruptions that inhibit ovulation.
Underweight: Can result in insufficient estrogen production, preventing ovulation.
Obesity: Can cause hormonal imbalances that affect ovulation, such as increased insulin resistance or elevated estrogen levels.
Conditions like diabetes, adrenal disorders, or autoimmune diseases can impact hormonal regulation and ovulatory function.
Certain medications, including hormonal contraceptives, antidepressants, and steroids, can interfere with normal ovulation.
As women age, the quality and quantity of eggs decline, leading to irregular ovulation and reduced fertility.
Diagnosing ovulatory dysfunction involves a detailed medical history, physical examination, and targeted blood and ultrasound investigations to identify the underlying cause.
Accurate diagnosis is crucial, as effective treatment options are tailored to address the specific cause of ovulatory dysfunction, enhancing the chances of restoring normal ovulation and achieving pregnancy.

For individuals with weight-related hormonal imbalances, achieving a healthy weight through diet and regular exercise can restore ovulation. Managing stress and avoiding excessive exercise or restrictive diets also supports hormonal balance.
Ovulation Induction (OI) refers to the use of medication to stimulate follicle growth and facilitate ovulation. The medication used in OI will be determined by the underlying cause. Medications may be oral (Letrozole or Clomiphene) or subcutaneous injections (FSH):
Letrozole and Clomiphene are commonly prescribed for women with Polycystic Ovarian Syndrome (PCOS). These oral medications work by prompting the pituitary gland to increase the release of FSH, which stimulates the growth of ovarian follicles.
Both medications are taken for five days, after which the rise in FSH stimulates a follicle to grow and prepare for ovulation.
FSH injections are often used when ovulation issues stem from inadequate signaling between the brain and the ovaries. They may also be prescribed for women with PCOS in certain cases. These injections directly stimulate the ovaries to grow follicles and support ovulation.
One of the main challenges of OI is controlling the development of a single follicle. Without careful monitoring through hormonal blood tests and ultrasounds, there is a risk of multiple pregnancies. To minimise this risk, couples are advised to abstain from unprotected intercourse until they are informed it is safe.
Ovulation will either occur naturally or with the aid of a ‘trigger’ injection to ensure proper timing. The luteal phase (the second half of the cycle) is often supported with progesterone to enhance the chances of successful implantation. The goal of OI is to provide monthly opportunities for conception based on the woman’s age and overall fertility health.
For further information on Ovulation Induction:
For those trying to conceive, fertility treatments like ovulation induction or assisted reproductive technologies, including IVF, can be considered. IVF involves stimulating the ovaries to produce multiple eggs, which are retrieved, fertilised in a lab, and transferred to the uterus.

While not all cases of ovulatory dysfunction can be prevented, especially those related to genetic or medical conditions, certain lifestyle and health practices can reduce the risk and support regular ovulation. Some key considerations are:

If you are experiencing any of the signs of Ovulatory Dysfunction or have concerns about your reproductive health, then seeking help early is key. By addressing any underlying causes, we can work together on a personalised treatment plan that will help to restore normal ovulation with the goal of achieving a pregnancy.
Common causes include PCOS, thyroid disorders, hyperprolactinemia, premature ovarian insufficiency (POI), stress, excessive exercise, and poor nutrition.
Irregular or absent ovulation makes conception difficult as no egg is available for fertilization.
Diagnosis involves:
Yes. Maintaining a healthy weight, managing stress, and addressing underlying medical conditions can improve ovulation.
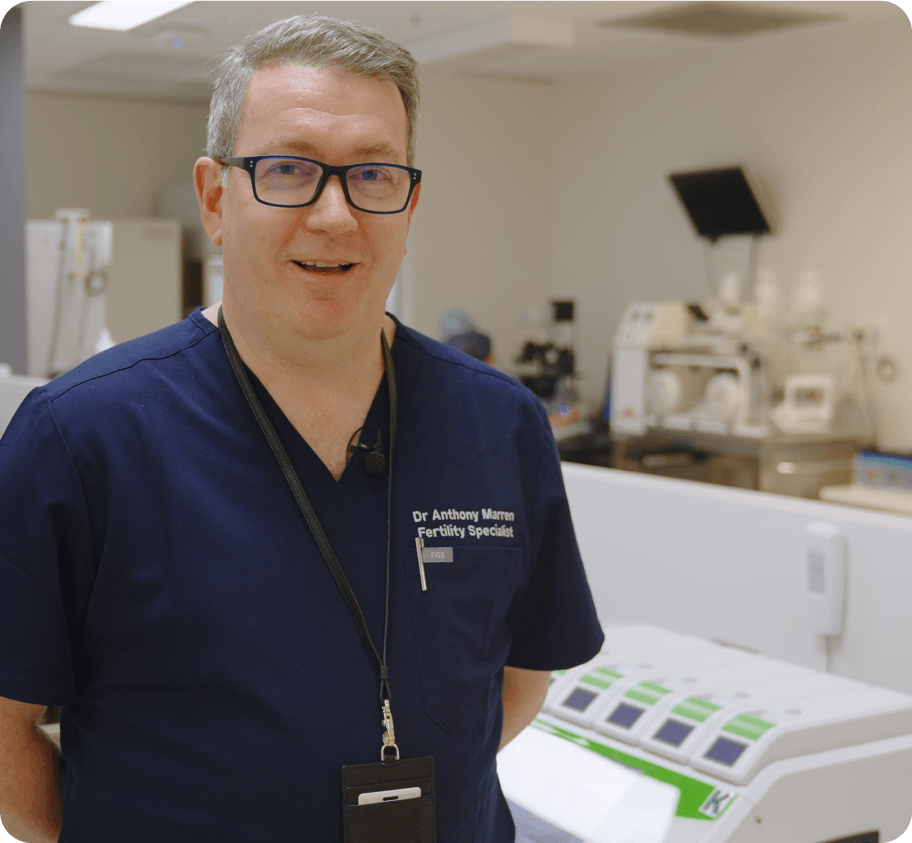
Yes. Dr. Anthony Marren specializes in ovulatory dysfunction diagnosis and treatment, offering personalized fertility solutions.